Intelligent Automation Products, Proven Outcomes
Claim Denials AI Management
Claims Denials management is critical for healthcare providers to optimize revenue and reduce financial leakage caused by claim denials. We combine the approach of using Claims Data to identify denials patterns by using AI and Machine Learning; our automations can invoke automations pre-submission and post denial.
Using the following data sources, we can get all the information needed to predict and provide confidences on why the claim might be denied or why it was denied.
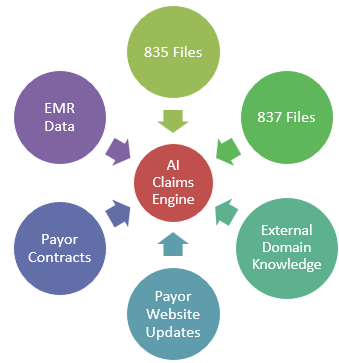
Using AI and Automation the AI Engine can provide real time feedback as to the health of a Claim being submitted or appealed. Both public and private Payor are continuously changing their coverages. The AI Engine is updated with any downgrades of CPT codes or plan changes. In addition, it continues to refresh its data sources so trends can be identified and put in the hands of the team who are submitting these claims.
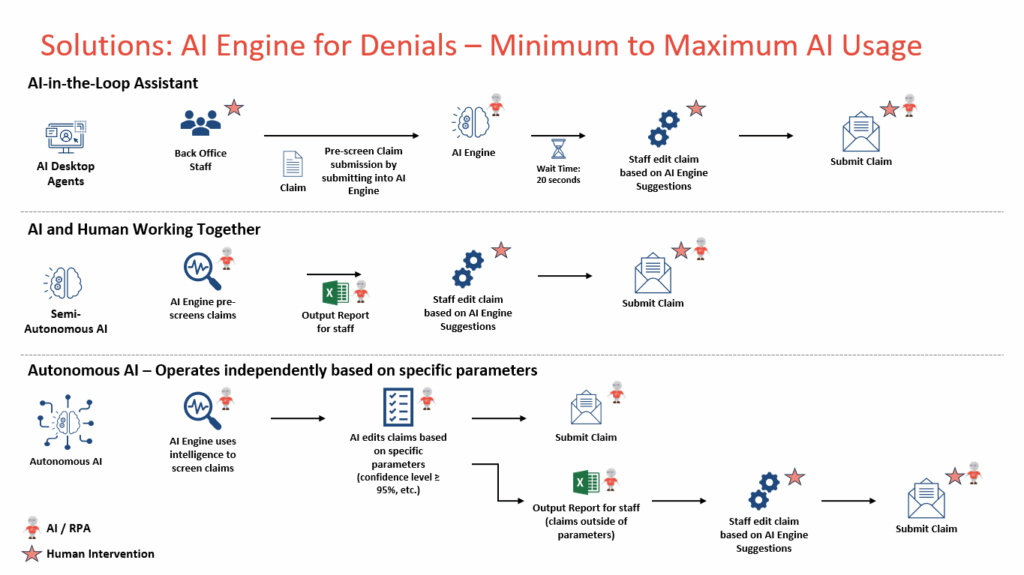
There are three different tracks for the implementation of the Claims AI Engine. All can be used together or separately. This allows the solution to scale to serve each workflow and provide as much complexity as possible.
Check out this solution in action!
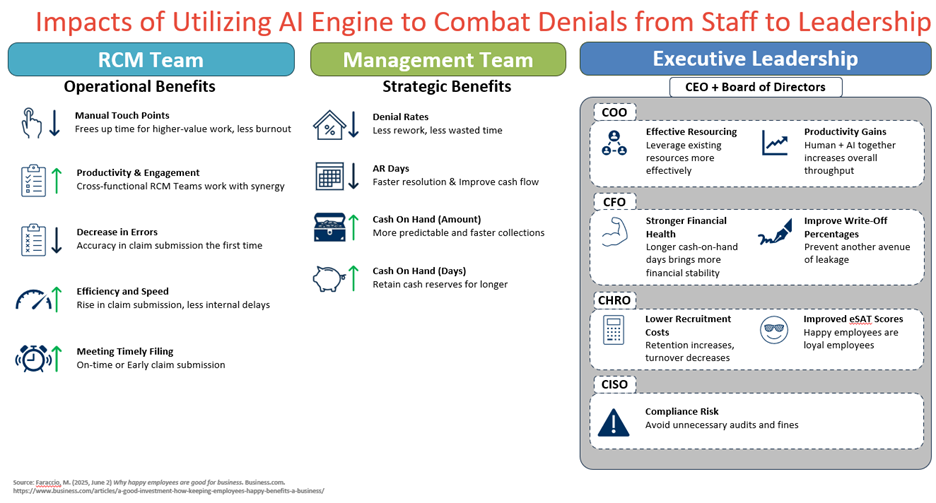
Some outcomes expected from the solution are the following: